
Ready, study, go!
Start your studies top informed.

Study your dream!
All information about studying.

Stay in touch!
Stay connected with the university.

Study with Purpose!
Discover our study programmes.

Educate with Purpose!
Lifelong learning and thinking ahead.
Research with Purpose!
Research from idea to application.

Better together!
As a university we create new opportunities.
Josef Ressel Centre Management
Contact
Josef Ressel Centre for research into predisposition to perinatal metabolic programming of obesity
FH JOANNEUM
Eggenberger Allee 11
8020 Graz
T: +43 316 5453 – 6612
E: info.jrp@fh-joanneum.at
Funding providers / Partners
Nutricia Milupa GmbH is a funding and expert partner to the Josef Ressel Centre for research into predisposition to perinatal metabolic programming of obesity.
The company celebrates its 60th anniversary in Austria this year and is the leading expert in nutrition for the first 1000 days. For over 40 years it has worked at its own breastfeeding research centre, the Nutricia Research Centre in Utrecht, to discover the ideal form of nourishment from the start of pregnancy through to early childhood, acknowledging that the gold standard, breast milk, can never be achieved by industrial means.
Other FH JOANNEUM institutes involved
Literature
WHO (2013). Vienna Declaration on Nutrition and Noncommunicable Diseases in the Context of Health 2020. WHO Ministerial Conference on Nutrition and Noncommunicable Diseases in the Context of Health 2020. Vienna: 4 – 5 July 2013.
WHO (2016). Report of the Commission on Ending Childhood Obesity, WHO 2016, ISBN 978 92 4 151006 6.
WHO (2016). Good maternal nutrition. The best start in life. Denmark: WHO Regional Office for Europe.


What is the link between obesity and early childhood nutrition? The Josef Ressel Centre for research into predisposition to perinatal metabolic programming of obesity is examining this key question. The JR Centre based at the Institute of Midwifery at FH JOANNEUM is a programme of excellence supported by the Christian Doppler Research Association for a period of five years. The research centre receives funding from the Federal Ministry of Science, Research and Economy (BMWFW) and the industrial partner Nutricia Milupa Austria.
The onset of obesity is one aspect of this wide-ranging research project. Research focuses on the first 16 weeks of life and examines any potential difference in the volumes ingested by breastfed babies and those fed on formula. Even in these early weeks of life, dietary behaviour can shape an irreversible metabolic trend leading towards the onset of obesity. In subsequent research periods up to the age of two, children are again examined according to further anthropometric, biophysical, biochemical and clinical parameters linked to the onset of obesity.
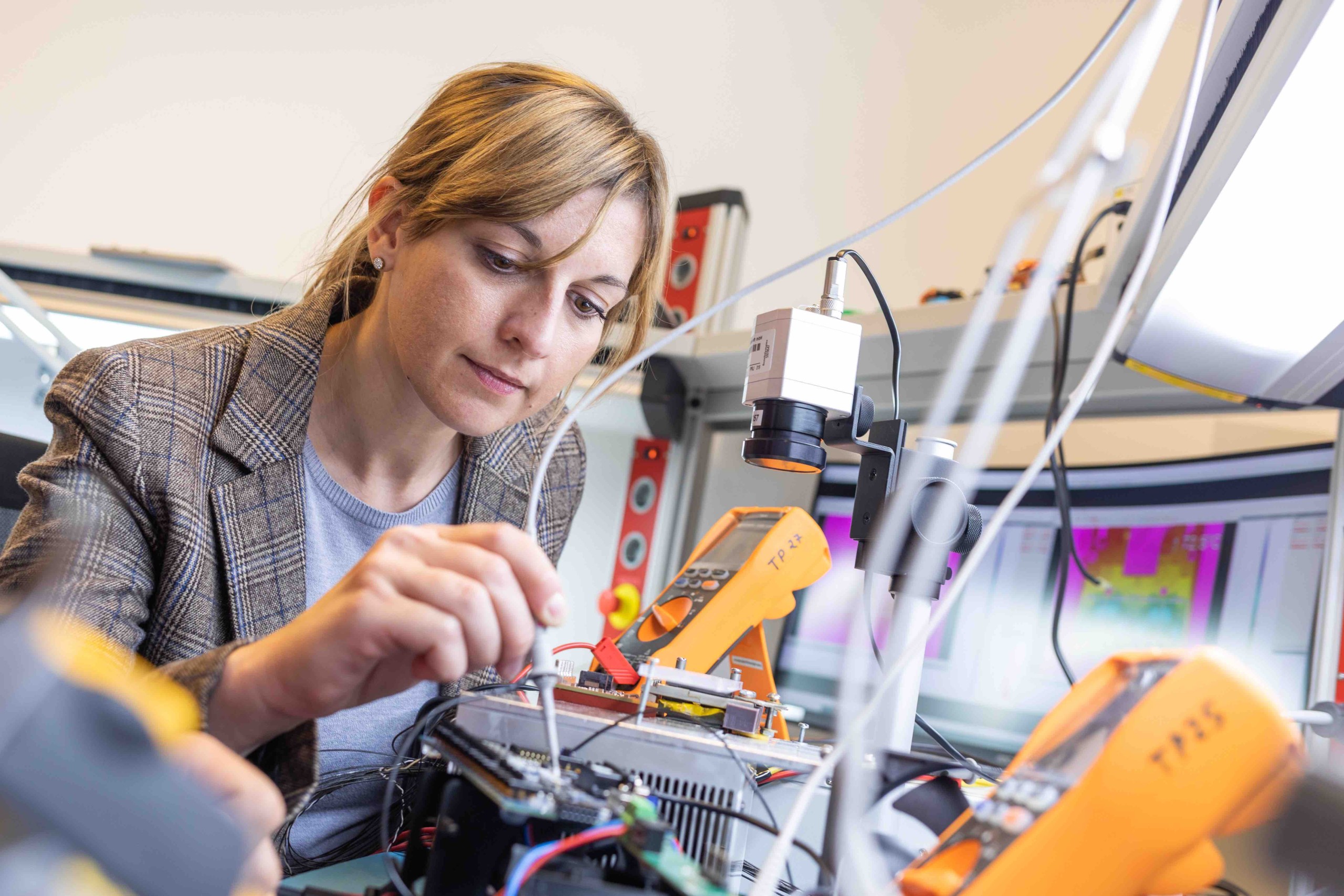
What makes this research so innovative is the focus it places on the very first phase of life, from pregnancy to two years of age, with the mother and child unit monitored using a range of measures. Consequently, the approach is strongly interdisciplinary, with experts in the fields of midwifery, medicine, care, nutrition, psychology, biomedical science and IT using state-of-the-art technology to examine the subjects.
Research focus. Research aims.

Foto: FH JOANNEUM
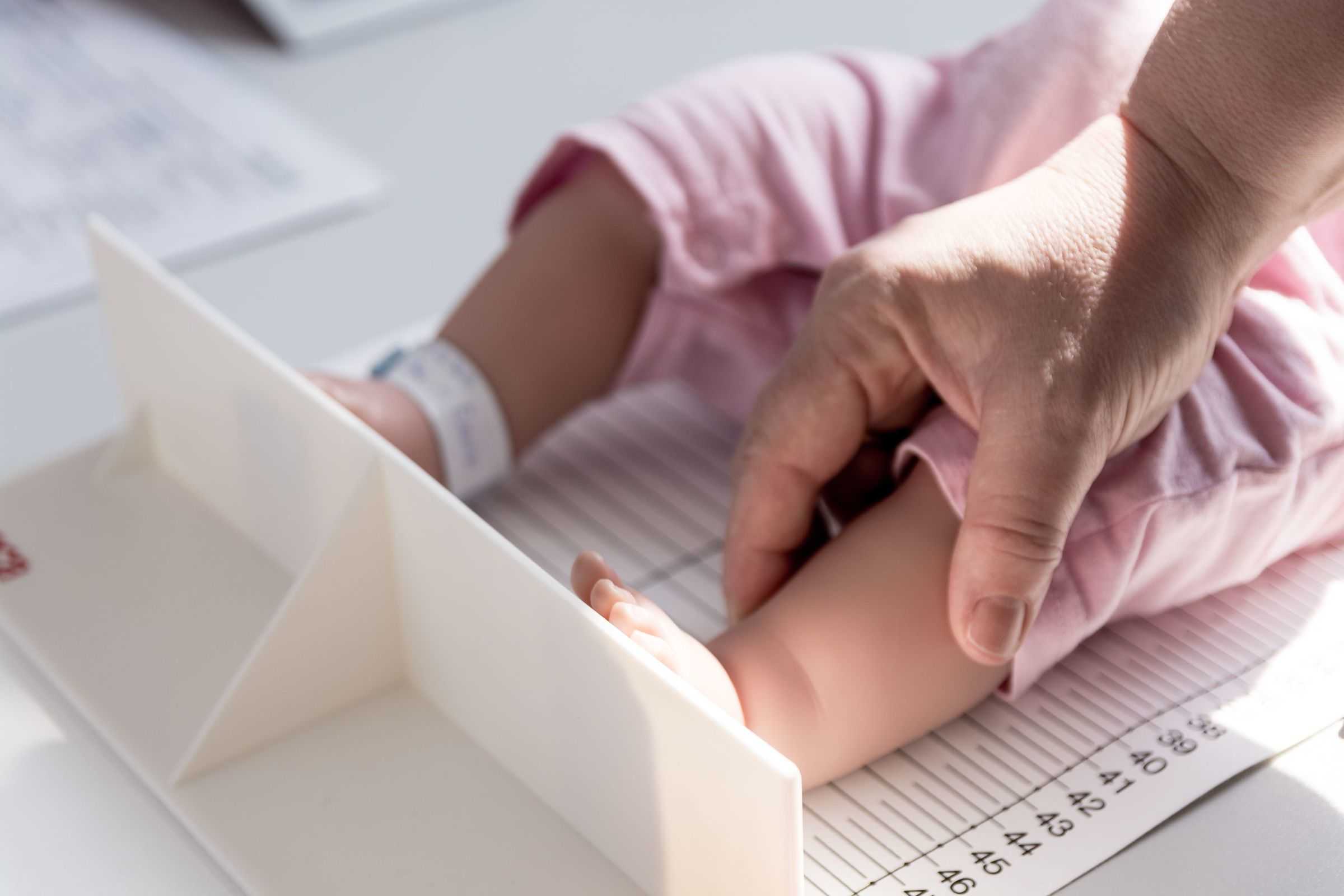
Foto: FH JOANNEUM / David Jablonski

Foto: FH JOANNEUM

Foto: FH JOANNEUM / David Jablonski

Foto: FH JOANNEUM / Maximilian Thum

Foto: FH JOANNEUM / Manfred Terler
The first 1000 days.
Measuring satiety signals
One of the hypotheses used to explain metabolic programming is the significant role played by overfeeding in the pre- and post-natal period. However, “overfeeding” has not been defined in either qualitative or quantitative terms. For example, overfeeding can be seen in terms of volume ingested, ingredients, or perception of satiety. In terms of the number and frequency of feeding times, precise monitoring of the volumes ingested by breastfed children and those fed on formula can provide information on its impact on patterns of growth and associated body fat mass.
Children who have been bottle-fed, whether with formula or their own mothers’ milk, are at a greater risk of being overweight in later life. Encouraging a child to drink too much is a major factor, and one which is magnified where the baby’s signals of satiety are ignored. Consequently, one aim of the project is to identify patterns of sucking, pulse, oxygen saturation and muscle tone which can be recognised by mothers as clear signals of satiety. This, in turn, helps prevent overfeeding.
Recording the volume ingested
The volume ingested and the associated intake of macro- and micro-nutrients is relevant. Excessive feeding, particularly of macro-nutrients, leads to an oversupply of nutrients to the developing child. Hence recording the volume ingested is a further important objective of the research project.
Tracking growth
Another aim of the research is to track the growth of children over their first two years of life in order to identify clear indicators for the development of excess weight as it relates to feeding styles. A particular focus is placed on how body fat accumulates, as fat cells in adipose tissue function as ductless glands which have a significant impact on the development of the organism.
Overfeeding in the first 16 weeks of life results in faulty programming of the hormone axes and this, in turn, has a decisive impact on future human health. The biological path towards obesity and its associated secondary subacute diseases appears to be established where negative factors cause adipose tissue to develop atypically.
Identification of molecular processes
Relevant biomarkers in different biological samples taken from mother and child are established as a means of identifying processes at physiological and molecular levels. Measurements include hormones relating to the energy budget and stress balance as well as satiety hormones and inflammation parameters. The microbiome is also recorded, as the composition of intestinal flora has a significant influence on human development.
The findings from the anthropometric data—such as BMI, body fat mass and growth trajectories—and the nutritional questionnaires are compared with the molecular factors. This is designed to highlight potential correlations with styles of feeding in order to identify molecular processes which lead to obesity.
To access the youtube video, click the button below. Please note that doing so will share data with third-party providers.
Innovative nature of the research.
At present there is no evidence-based data on the actual volume intake and feeding behaviour of babies fed on formula compared with those who are breastfed. This study breaks new ground by examining connections between the volumes ingested and the babies’ rate of growth, together with an analysis of body composition—the proportion of fat—and an analysis of the macronutrients and calorific value of mothers’ milk. Another novel aspect is the longitudinal design of the research. The study includes children who are born healthy and at full-term.
Relevance of the research.
According to World Health Organisation studies (WHO 2013), the global prevalence of obesity has tripled since the 1980s. In Austria, for example, during the period from 2008 to 2012 the proportion of obese girls increased from 10% to 16%, and boys from 12% to 17% (BMG, 2012). Being overweight is a risk factor for obesity, and this in turn leads to many serious secondary diseases. Today obesity is the fifth largest risk factor for premature death. An effective prevention strategy is a significant determinant in successfully fighting this trend. New strategies are being followed, including the development and implementation of health and support programmes during and after pregnancy (WHO, 2016).
The onset of obesity is caused by many factors and is by no means completely understood. However, nutrition in early childhood has an important impact on metabolism. Both overfeeding and a lack of nutrition in the foetal period—measured by low and high birthweight—and in early childhood contribute to the onset of obesity and type 2 diabetes.
During the phase in pregnancy and after birth in which the organs are rapidly developing and differentiating, metabolic and other factors can exert long-term effects on the function of the organism in later life. This phenomenon is termed perinatal metabolic programming or metabolic imprinting. The first 1000 days include the period from conception to two years of age. This period of time is seen as a sensitive phase of metabolic development.



